Alopecia areata and seborrheic dermatitis are immune-driven skin disorders linked to micronutrient deficiencies and gut-skin imbalance, with conventional therapies offering only temporary relief. A 21-year-old male underwent a three-month functional nutrition protocol combining an elimination diet, nutraceuticals, and topical support, resulting in biochemical normalization, hair regrowth, reduced dermatitis, improved digestion, energy, sleep, and overall skin health. This case shows how a root-cause-focused functional nutrition protocol with targeted supplementation can support recovery in immune-related skin conditions.
Alopecia areata is an autoimmune disorder marked by sudden hair loss on the scalp or body, appearing as patchy bald spots or diffuse thinning. Since follicles remain intact, regrowth is possible¹. Immune dysfunction involving plasmacytoid dendritic cells, NK cells, T cells, and cytokines such as interferon-γ, IL-15, IL-23, and IL-32, alongside genetic and environmental triggers, contributes to pathogenesis²⁻⁴. Conventional treatments, including steroids, immunotherapy, oral minoxidil, PRP, and transplants, often provide limited or temporary results with risks such as hypertension, headaches, cardiac issues, allergic reactions, and relapse⁴⁻⁵.
Seborrheic dermatitis is a chronic inflammatory condition affecting sebaceous-rich areas like the scalp, face, and chest⁶⁻⁸. It stems from immune hypersensitivity to Malassezia species, aggravated by excess sebum and impaired barrier function⁷⁻⁸. Symptoms include red, greasy, itchy, flaky patches⁶⁻⁷. Conventional therapies, antifungals, corticosteroids, salicylic acid, selenium sulfide, and botanicals like tea tree oil, offer only symptomatic relief⁸.
Functional nutrition targets immune dysregulation, gut imbalance, inflammation, and nutrient deficiencies through advanced testing, dietary modulation, and supplements such as zinc, vitamin D, and adaptogens⁹⁻¹⁰. This case highlights functional nutrition as a supportive strategy for alopecia areata and seborrheic dermatitis in a 21-year-old male.
A 21-year-old male from West Bengal, India, presented with patchy scalp and body hair loss, 40% eyebrow loss, scattered beard growth, and inflamed leg follicles. Seborrheic dermatitis had worsened after COVID-19 vaccination, and alopecia had been previously treated with a four-month course of tofacitinib, giving only temporary relief. Other complaints included fatigue, poor concentration, bloating, constipation, dry skin, recurrent ulcers, dandruff, nail patches, acne, and irregular sleep, leading to early retirement from professional chess. At baseline, his height was 194 cm and his weight was 70.95 kg. His diet was predominantly rice, eggs, chicken, and mutton.
Initial blood work revealed infection, inflammation, and metabolic dysregulation (Table 1). To further evaluate root causes, advanced testing was performed. GI-MAP showed gut dysbiosis with reduced commensals and elevated β-glucuronidase. Array 12 revealed immune reactivity to mould (Stachybotrys chartarum) and Klebsiella. OMX highlighted amino acid imbalances.
A root-cause-based protocol was initiated, eliminating gluten, dairy, sugar, and seed oils, and introducing whole foods, coconut-based smoothies, and anti-inflammatory herbs. Supplements included magnesium glycinate, vitamin D3 + K2, B-complex, zinc, probiotics, omega-3 krill oil, CoQ10, biocidin, digestive enzymes, immunoglobulins, Akkermansia, camu camu, glutathione, and branched-chain amino acids. Topical tea tree oil was used for dermatitis, and castor oil for eyebrow regrowth. Lifestyle optimisation focused on sleep, strength training, and hydration.
By April 2025, follow-up showed significant biochemical improvements in vitamin D, homocysteine, insulin, and inflammatory markers (Table 1). Clinically, the patient reported eyebrow regrowth, reduced dandruff and flaking, improved digestion, deeper sleep, higher energy, weight gain of 2.1 kg, and improved concentration. Continuation of a personalized diet protocol was recommended to sustain recovery.

At presentation, baseline serum parameters (Table 1) showed markedly elevated homocysteine (23.2 µmol/L), indicating Vitamin B6 and Folate deficiency linked to dermatitis. Ferritin was high (262 ng/mL), suggesting systemic inflammation. Vitamin D was severely low (9.12 ng/mL), likely contributing to fatigue, dry skin, poor immune regulation, and autoimmunity. Elevated SGPT and SGOT suggested liver damage, possibly gut-driven.
Advanced functional testing was conducted for unresolved gut and autoimmune symptoms.
GI-MAP revealed reduced commensals, with Akkermansia muciniphila and Faecalibacterium prausnitzii undetectable. Core phyla Bacteroidetes (9.38e10) and Firmicutes (3.70e8) were below limits, reducing diversity. β-Glucuronidase was high (3705 U/mL), impairing detoxification. Secretory IgA was low (372 µg/g). OMX showed elevated phenylalanine (139.9 nmol/mL), suggesting impaired amino acid metabolism and liver stress. Low isoleucine, valine, threonine, and glycine further indicated compromised protein utilisation. Due to high phenylalanine, branched-chain amino acids (BCAA) were selected instead of essential amino acids (EAA).
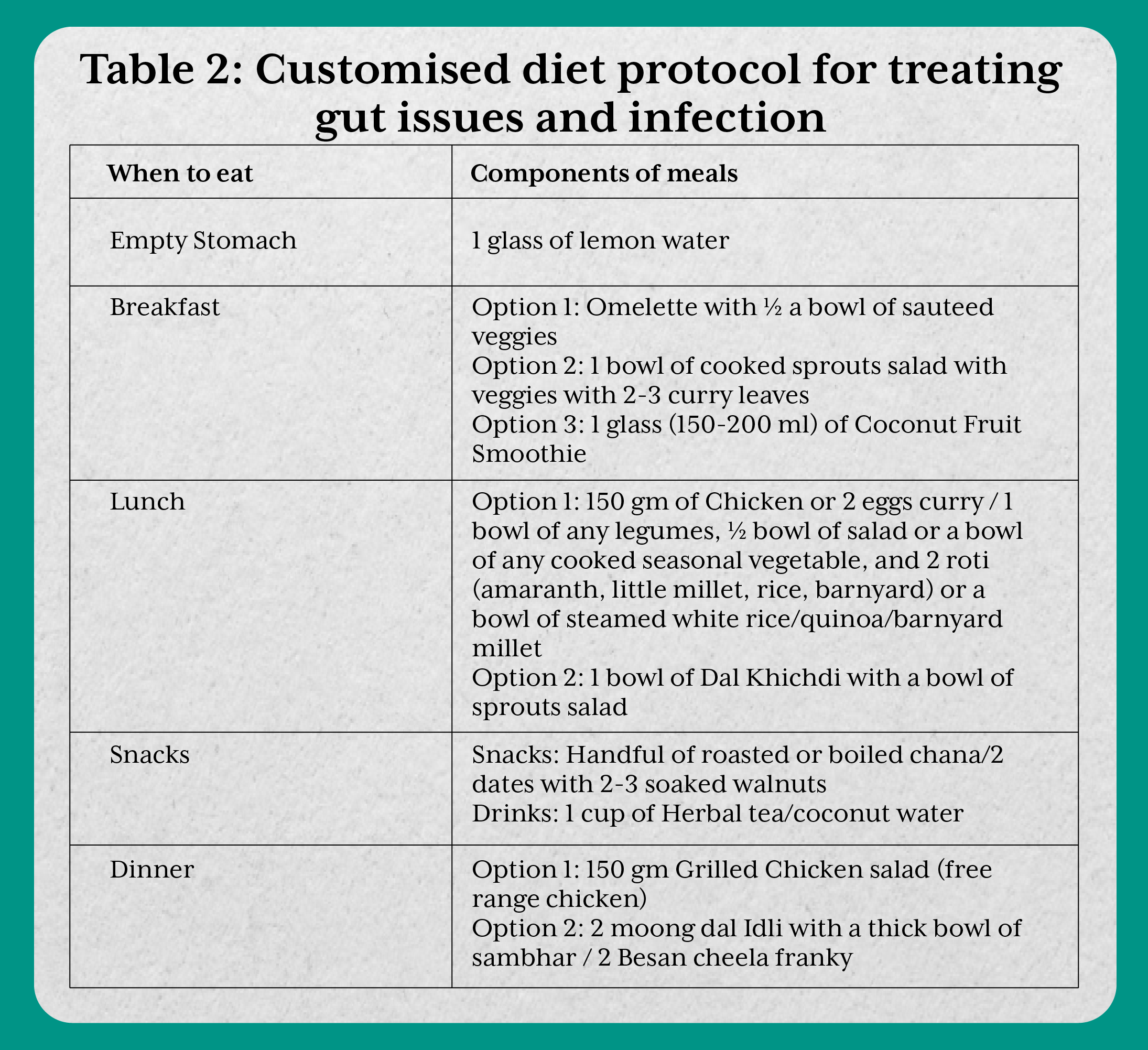
He was prescribed an anti-inflammatory diet (Table 2) excluding red meat, gluten, dairy, and seed oils, with emphasis on clean proteins (chicken, eggs), low-glycemic carbs (millets, rice, quinoa), seasonal vegetables, and antioxidant-rich foods (berries, dragon fruit). Carbohydrates, previously dominant, were reduced to improve insulin sensitivity, with higher-quality proteins added. Garlic, ginger, and lemon supported detoxification and gut balance. Meals were cooked in ghee, butter, or coconut oil, avoiding industrial oils. The structured plan targeted digestion, circadian rhythm, glycemic control, and detox pathways.
A three-month supplement protocol supported gut repair, immunity, and skin health. Core supplements included magnesium, vitamin D3+K2, B-complex, zinc, probiotics, omega-3 krill oil, Coenzyme Q10, digestive enzymes, camu camu, glutathione, biocidin, and BCAA. For skin, diluted tea tree oil resolved dermatitis within a month, castor oil stimulated eyebrow regrowth, and a glycerin-lemon mix supported hydration. Lifestyle advice emphasised strength training, restorative sleep, and hydration.
After 3 months, labs showed vitamin D improved from 9.12 to 49.96 ng/mL, homocysteine dropped from 23.2 to 16.35 µmol/L, insulin and glucose improved, ferritin decreased (262 → 222.7 ng/mL), and liver enzymes trended down. Bilirubin fell from 1.55 to 0.92 mg/dL, reflecting improved detoxification. Clinically, the patient reported visible baby hair regrowth within 6 weeks, 2.5 kg weight gain, complete resolution of bloating, constipation, and gas, improved energy, and a consistent sleep routine (asleep by 11 PM). Seborrheic dermatitis resolved by the first month with tea tree oil, castor oil supported eyebrow regrowth, mouth ulcers became infrequent, and overall skin hydration and tone improved.
A 2020 pediatric case study reported full hair regrowth within five months in a child with patchy alopecia areata after starting a whole-food diet with probiotics and omega-3 supplements¹¹. Although our patient was an adult with additional seborrheic dermatitis, both cases show that nutritional support and microbiome modulation may aid immune-mediated hair recovery without pharmacologic interventions.
Seborrheic dermatitis has also been linked to diet. A 2024 case–control study found that individuals with seborrheic dermatitis had significantly lower antioxidant intake and higher glycemic load compared to controls, promoting oxidative stress and inflammation¹². In our case, transitioning to a low-glycemic, anti-inflammatory nutrition plan reduced flaking and itching, aligning with recent literature.
A 2024 pilot study explored a probiotic-enriched topical formulation for seborrheic dermatitis and observed rapid symptom improvement with microbiome modulation¹³. Similarly, probiotics were included here to support microbial balance, alongside topical tea tree oil in coconut oil to reduce inflammation and flaking, and castor oil for eyebrows, which showed visible regrowth within weeks.
This case highlights how a functional nutrition protocol can yield sustainable improvements in relapsing immune-related skin conditions, with tailored dietary changes and targeted supplementation producing more durable outcomes than conventional therapies.
Written consent was obtained from the patient to publish the case report.