Introduction
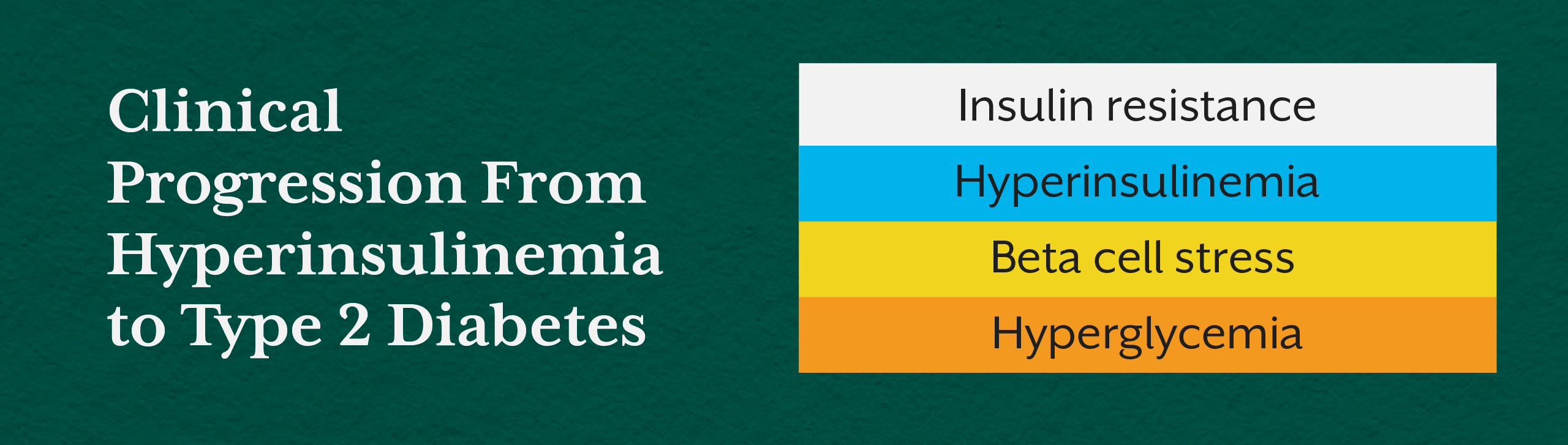
In clinical practice, type 2 diabetes is often identified by elevated fasting glucose or HbA1c. However, these markers represent the final stage of metabolic failure, not its beginning. Long before glucose levels rise, many individuals experience a prolonged phase of chronically elevated insulin, a condition known as hyperinsulinemia.
Hyperinsulinemia reflects the body’s attempt to maintain normal blood glucose in the face of worsening insulin resistance. During this phase, glucose values may still appear “normal,” masking the underlying metabolic strain. As a result, individuals are often reassured that their reports are fine, even while fatigue, weight gain, cravings, and energy crashes quietly intensify.
From a functional and systems-based perspective, hyperinsulinemia is not a side effect of diabetes. It is one of the primary hidden causes of type 2 diabetes and a critical clinical signal that demands early recognition.
Understanding Hyperinsulinemia Beyond Glucose Values
What Is Hyperinsulinemia?
Hyperinsulinemia refers to persistently high insulin levels in the blood, typically as a compensatory response to insulin resistance. When cells become less responsive to insulin, the pancreas increases insulin secretion to keep glucose levels stable.
In early stages, this compensation is effective. Blood sugar remains within range, but insulin levels rise far beyond what is metabolically healthy. Over time, this chronic overstimulation places enormous stress on pancreatic beta cells and accelerates metabolic dysfunction.
Importantly, hyperinsulinemia can exist years before diabetes is diagnosed, making it one of the most under-recognized drivers of disease progression in conventional care.
Hyperinsulinemia Causes: Why Insulin Keeps Rising
Hyperinsulinemia does not arise from a single trigger. It is the cumulative outcome of metabolic overload, lifestyle stressors, and cellular dysfunction.
Chronic Insulin Resistance
As insulin resistance develops in muscle, liver, and adipose tissue, cells fail to respond effectively to insulin’s signal. The pancreas compensates by producing more insulin to overcome this resistance. Over time, this leads to sustained hyperinsulinemia.
Excessive Refined Carbohydrate Intake
Frequent consumption of refined carbohydrates and ultra-processed foods leads to repeated insulin spikes. Without sufficient recovery time, insulin remains chronically elevated, impairing receptor sensitivity and reinforcing resistance.
Visceral and Ectopic Fat Accumulation
Fat accumulation in the liver and pancreas interferes with insulin signaling and secretion. This mechanism plays a central role in the metabolic deterioration seen in prediabetes and type 2 diabetes.
Chronic Stress and Cortisol Dysregulation
Persistent stress elevates cortisol, which raises blood glucose through gluconeogenesis. This indirectly drives insulin secretion, contributing to chronically high insulin levels even in the absence of excessive carbohydrate intake.
High Insulin Levels Symptoms: Clinical Clues Often Missed
Hyperinsulinemia symptoms are often subtle and nonspecific, leading to underdiagnosis. Yet, when viewed collectively, they offer valuable insight into early metabolic dysfunction.
Common high insulin levels symptoms include persistent fatigue, difficulty losing weight despite calorie restriction, frequent hunger, sugar cravings, post-meal energy crashes, and central fat accumulation. Many individuals also report brain fog, mood instability, and disrupted sleep.
These symptoms are frequently dismissed or attributed to lifestyle stress, aging, or hormonal imbalance, rather than recognized as signs of metabolic compensation.
For a broader understanding of how early metabolic imbalance manifests clinically, readers may also find value in the iThrive Academy blog “Top Nutritional Mistakes That Damage Heart Health After 30,” which explores early metabolic strain well before diagnosis.
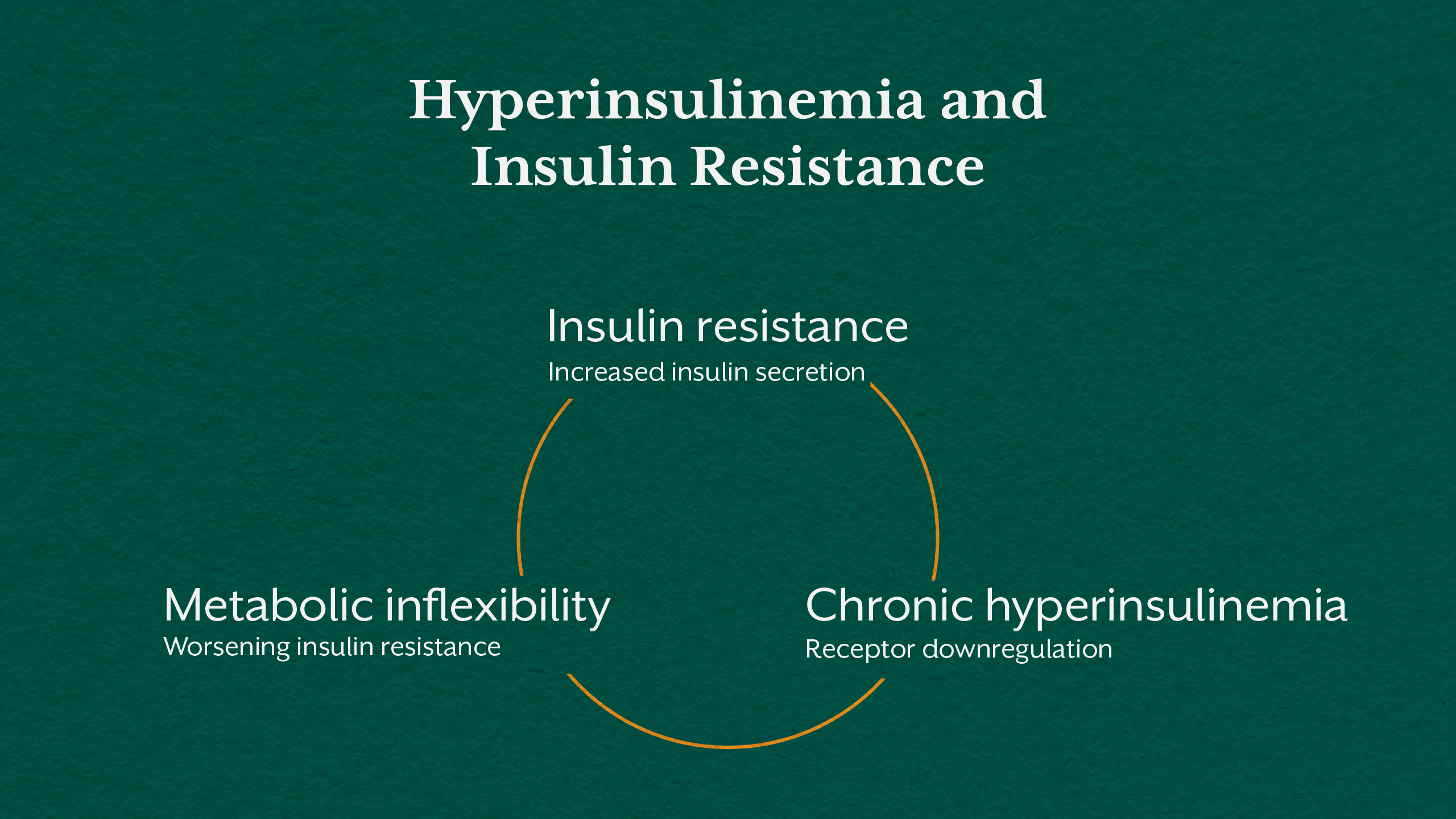
Insulin Resistance and Hyperinsulinemia: A Bidirectional Cycle
Insulin resistance and hyperinsulinemia reinforce each other in a vicious metabolic loop. As insulin resistance worsens, insulin secretion increases. As insulin remains elevated, receptor sensitivity further declines.
This cycle contributes to metabolic inflexibility, impaired fat oxidation, and increasing reliance on glucose metabolism. Over time, the pancreas begins to fatigue, leading to declining insulin output and rising blood glucose.
Understanding this relationship is critical in clinical practice. Treating glucose alone without addressing hyperinsulinemia perpetuates disease progression rather than reversing it.
Why Hyperinsulinemia Is a Hidden Cause of Type 2 Diabetes
Type 2 diabetes is diagnosed when insulin compensation fails. By this stage, years of hyperinsulinemia have already altered mitochondrial function, increased oxidative stress, and disrupted hormonal balance.
Because glucose remains normal during early compensation, standard screening fails to detect risk. This delay reinforces the misconception that diabetes appears suddenly, rather than emerging from long-standing metabolic strain.
If you want to explore how functional approaches assess chronic metabolic stress beyond conventional labs, the iThrive Academy blog “The Functional Nutrition Secret to Fat Burning That Mainstream Diets Don’t Want You to Know” provides additional context on metabolic flexibility and insulin dynamics.
Can Hyperinsulinemia Be Cured? A Clinical Perspective
Hyperinsulinemia is not a permanent condition. When identified early, it is modifiable and often reversible. However, reversal depends on addressing root causes rather than suppressing glucose.
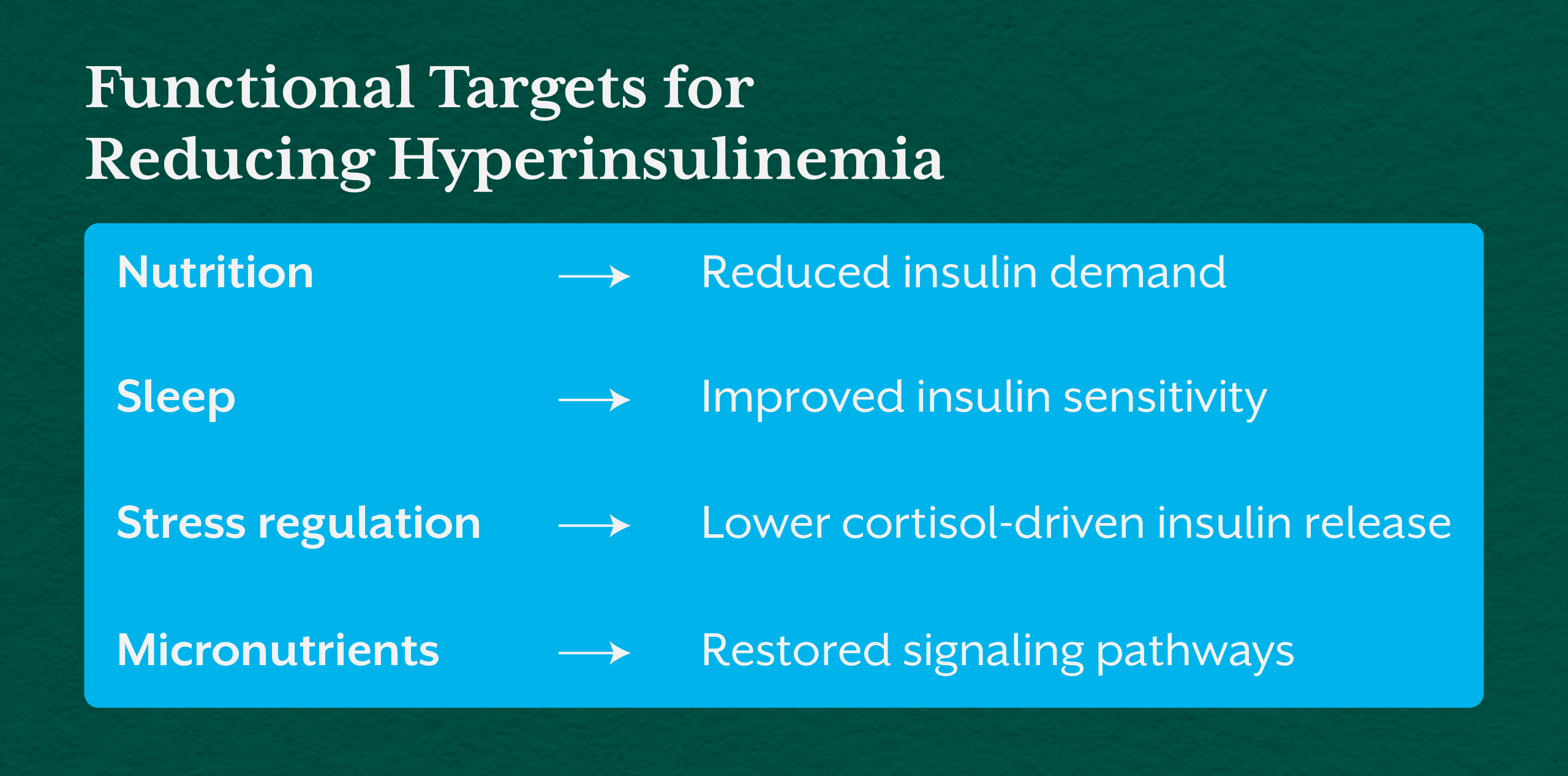
Effective hyperinsulinemia treatment focuses on improving insulin sensitivity, reducing metabolic load, restoring circadian rhythm, and supporting mitochondrial function. Nutrient sufficiency, particularly magnesium and B-vitamins, plays a critical role in improving insulin signaling and glucose oxidation.
Education that trains practitioners to identify and intervene during this early phase is essential. Programs such as the iThrive Certified Functional Nutrition Course emphasize systems-based assessment, helping clinicians move beyond glucose-centric care.
How to Fix Hyperinsulinemia: Principles, Not Protocols
Fixing hyperinsulinemia requires a shift from symptom suppression to metabolic repair. This includes reducing insulin demand through dietary restructuring, improving sleep and circadian alignment, managing stress, and correcting micronutrient deficiencies.
Importantly, interventions must be individualized. What lowers insulin demand for one person may worsen metabolic stress for another. This is why practitioner education grounded in physiology and systems biology is central to effective care.
Key Takeaway
Hyperinsulinemia is not a secondary concern in metabolic health. It is a primary driver of insulin resistance and one of the most overlooked contributors to type 2 diabetes. Long before glucose rises, the body signals distress through chronically elevated insulin, altered energy metabolism, and subtle yet persistent symptoms.
Recognizing hyperinsulinemia as an early, actionable clinical state reframes diabetes prevention entirely. It allows practitioners and individuals to intervene before irreversible damage occurs, shifting care from late-stage management to true metabolic restoration. Education rooted in physiology as well, such as that offered through iThrive Academy and the ICFN program, equips clinicians and individuals to identify these patterns early and change long-term outcomes meaningfully.






.jpg)