Introduction
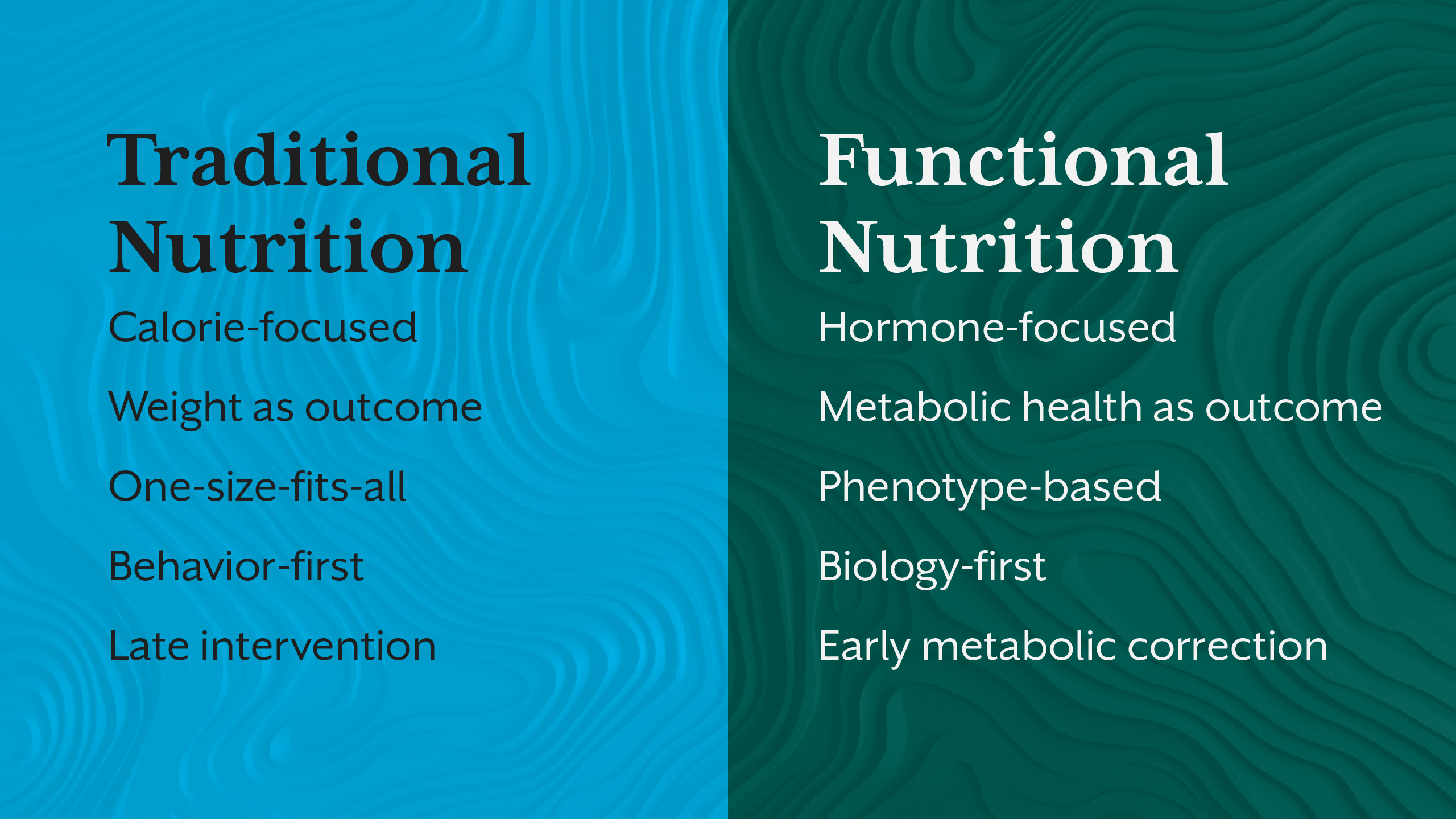
If you were trained in traditional nutrition education, chances are obesity was explained to you in a familiar way: people eat too much, move too little, and gain weight. Calories in, calories out. Behaviour change.
On paper, it sounds logical. In practice, it fails clinically, biologically, and educationally.
Obesity rates have continued to rise globally despite decades of calorie-focused dietary guidelines, food pyramids, and lifestyle counselling models. Yet nutrition curricula across universities, certification programs, and even continuing education still teach obesity as a willpower problem, not a systems-level metabolic condition.
This gap between obesity science and obesity education is not a minor oversight. It fundamentally shapes how practitioners assess clients, design interventions, and judge outcomes. More importantly, it limits how deeply learners understand the real causes of obesity, reinforcing outdated misconceptions that no longer align with current metabolic research.
This blog is an invitation to unlearn, not because traditional nutrition is “wrong,” but because it is incomplete.
The Calorie Model - Useful, But Not Sufficient
Traditional nutrition education treats obesity as a straightforward energy imbalance: sustained caloric excess leads to fat storage. This framework assumes that the body is a passive container where energy accumulation follows simple arithmetic.
But the human body is not a spreadsheet.
Calories do not exist in isolation. They are processed through hormones, enzymes, neural circuits, immune signals, and circadian rhythms. Two individuals consuming the same caloric intake can experience vastly different fat accumulation, appetite responses, and metabolic adaptations.
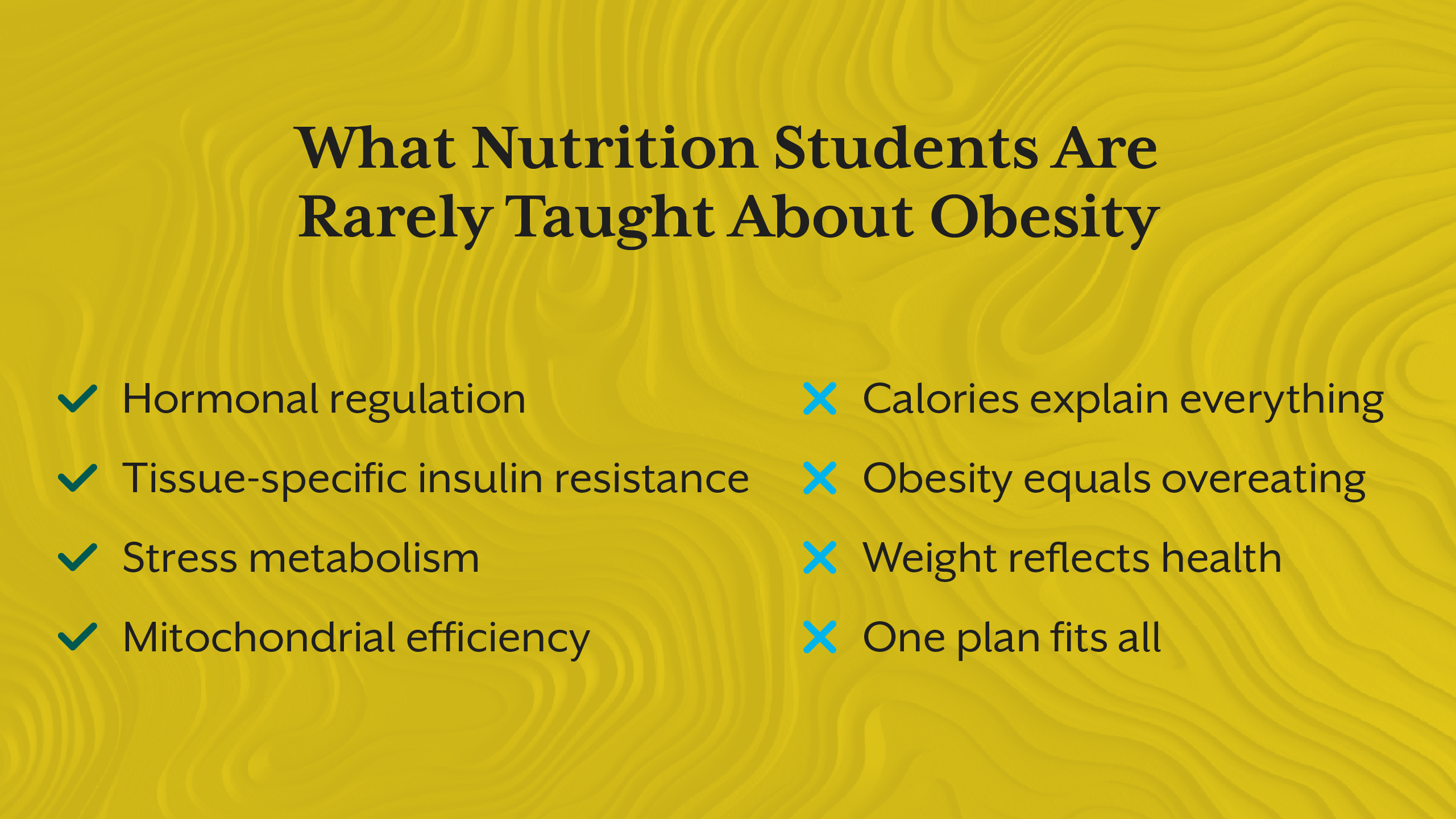
Modern obesity science shows that energy balance is regulated, not merely accounted. Hormones like insulin, leptin, cortisol, thyroid hormones, and gut peptides dynamically influence how calories are stored, burned, or conserved. When these systems are dysregulated, calorie reduction alone often triggers compensatory responses like increased hunger, reduced energy expenditure, and metabolic slowdown.
This is why many individuals experience weight regain despite strict adherence to hypocaloric diets. Traditional nutrition education rarely teaches these adaptive mechanisms in depth, leaving practitioners unprepared to explain why “doing everything right” still doesn’t work for many clients.
Obesity Is Taught as a Behaviour Problem - Not a Biological One
Another major flaw in obesity education is the overemphasis on behaviour without sufficient biological context. While eating patterns, physical activity, and lifestyle choices matter, they are often downstream expressions of metabolic state, not the root cause.
For example, insulin resistance alters fuel partitioning, pushing energy toward storage even when caloric intake is modest. Leptin resistance disrupts satiety signalling, making appetite regulation biologically harder, not psychologically weaker. Chronic stress elevates cortisol, preferentially increasing visceral fat deposition and glucose output.
When these mechanisms are not taught, obesity becomes moralised. Clients are labelled as “non-compliant,” “unmotivated,” or “undisciplined,” when in reality their physiology is resisting weight loss as a survival response.
This is explored further in the iThrive Academy blog “Insulin Resistance as a Pre-Diagnostic State: Why Type 2 Diabetes Is a Late Label”, which reframes metabolic dysfunction as an adaptive process long before disease thresholds are crossed.
Traditional nutrition education often fails learners by not teaching why behaviour change becomes harder as metabolic dysfunction deepens.
Obesity Is Not One Condition, But We Teach It Like One
Obesity is often presented as a uniform diagnosis defined by BMI cut-offs. Yet obesity science increasingly recognises multiple phenotypes:
- Insulin-resistant obesity
- Stress-driven obesity
- Hypothyroid-associated weight gain
- Sarcopenic obesity
- Inflammatory and gut-mediated obesity
Traditional nutrition education rarely differentiates between these patterns. As a result, learners are trained to apply standardized diet plans to biologically diverse individuals.
This mismatch explains why some clients respond dramatically to carbohydrate reduction, while others worsen. Why some thrive on fasting, while others experience fatigue, hair loss, or hormonal disruption.
Without phenotype-based education, obesity remains oversimplified and intervention outcomes remain inconsistent.
Compensation - The Phase Most Curricula Ignore
One of the most critical yet under-taught concepts in obesity education is metabolic compensation.
Before metabolic failure, the body adapts. Insulin levels rise to maintain glucose control. Fat tissue expands to buffer excess energy. Appetite signals shift. Stress hormones increase glucose availability. From a survival standpoint, this is intelligent physiology.
From an educational standpoint, it creates blind spots.
Clients may present with normal glucose, “acceptable” lipid profiles, and stable weight, while underlying metabolic strain escalates. Traditional nutrition education often waits for overt pathology before intervention, missing the opportunity for early metabolic correction.
This compensatory phase is discussed in depth in the iThrive Academy blog “The Metabolic Infrastructure Model: Rethinking the Root Cause of Diabetes”, which aligns obesity with systemic metabolic adaptation rather than isolated weight gain.
Obesity Is a Systems Problem, Not a Single-Nutrient Problem
Traditional nutrition education often searches for a villain: fat, sugar, carbs, processed foods. While dietary composition matters, obesity cannot be reduced to a single nutrient narrative.
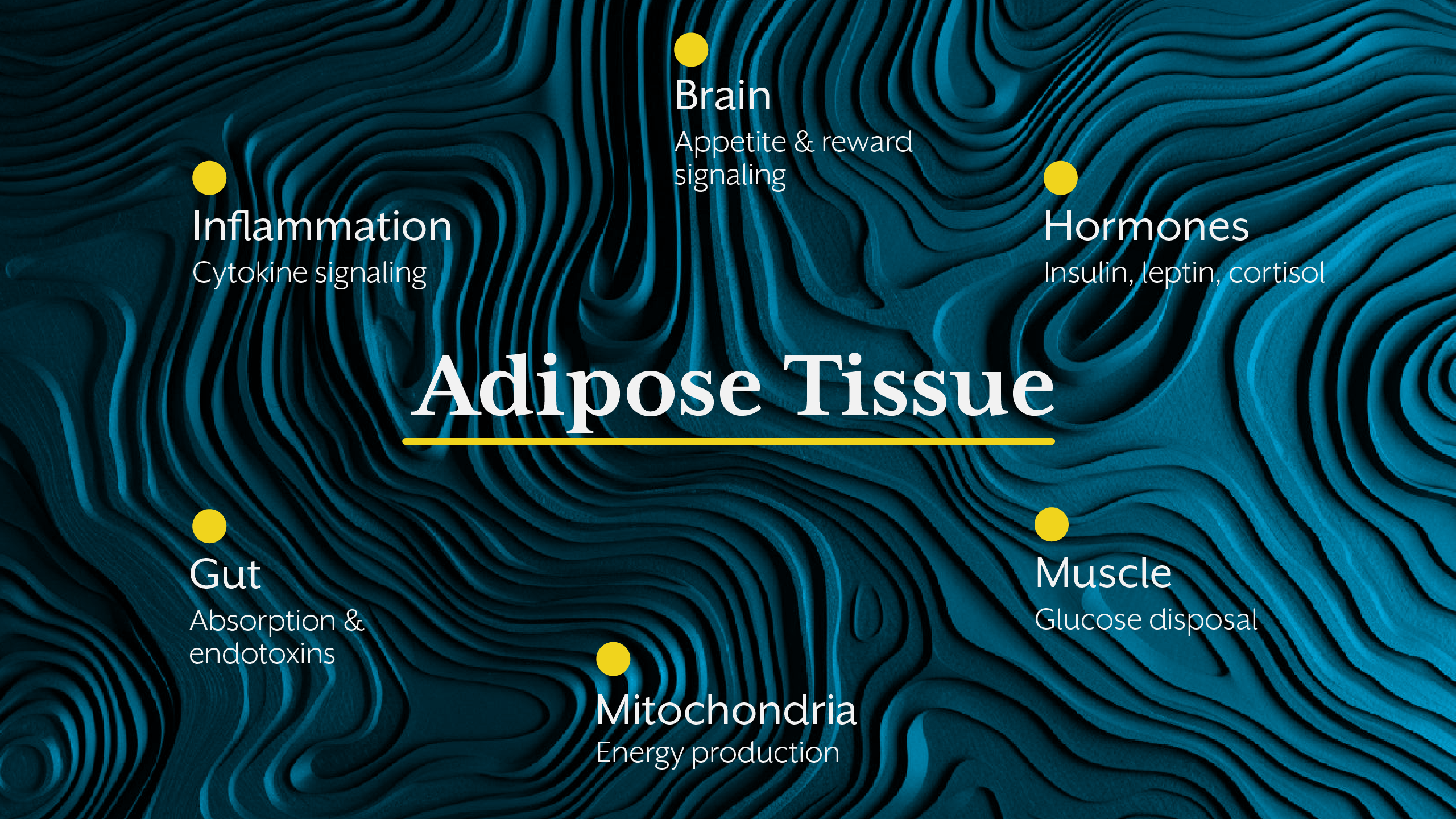
Obesity science highlights interacting systems:
- Energy-sensing pathways (AMPK-mTOR)
- Immune-metabolic crosstalk (JAK/STAT, cytokines)
- Neuroendocrine regulation (leptin-melanocortin axis)
- Circadian rhythm alignment
- Mitochondrial efficiency
When these systems are dysregulated, nutrient quality alone cannot override metabolic inertia. This is why advanced education must move beyond macros into metabolic infrastructure.
Programs like iThrive Certified Functional Nutrition (ICFN) are designed to train practitioners to assess and intervene at this systems level, bridging the gap between nutrition science and clinical outcomes.
Why This Gap Matters for Practitioners and Educators
When obesity is taught incorrectly, practitioners feel it in practice. Clients plateau. Results don’t sustain. Confidence erodes.
Many nutrition professionals quietly experience career frustration, not because they lack skill, but because their education didn’t equip them with modern obesity frameworks. This is one reason advanced, clinically-oriented education has become essential for practitioners seeking deeper credibility and better outcomes.
At iThrive Academy, obesity is taught not as a failure of discipline, but as a biological response to chronic metabolic stress - a perspective that empowers both learners and clients.
Re-Teaching Obesity - What Needs to Change
Obesity education must evolve from surface-level prescriptions to mechanism-based understanding. Learners should be trained to ask:
- What hormonal signals are dominant?
- Is the body defending weight through stress or inflammation?
- Is energy storage adaptive or pathological in this context?
This shift transforms obesity from a compliance issue into a solvable biological puzzle, one that requires skill, curiosity, and advanced training.
Key Takeaway
Obesity is not taught “wrong” because traditional nutrition lacks value, but because it stops too early. By reducing obesity to calories and behaviour, education overlooks the deeper biological intelligence driving fat storage, appetite regulation, and metabolic adaptation. Modern obesity science demands a systems-based, phenotype-aware, hormone-informed approach that equips practitioners to think beyond food charts and calorie targets. When we teach obesity correctly, we not only improve outcomes, we rather restore confidence, credibility, and clarity to nutrition education itself.






.jpg)