Introduction
If you work with thyroid patients long enough, you begin to notice a pattern that conventional frameworks struggle to explain.
Two patients walk in with nearly identical lab reports. Similar TSH. Similar free hormones. Similar antibody levels. Yet one improves rapidly with intervention, while the other remains symptomatic for years despite receiving what appears to be correct thyroid treatment.
This is the moment most practitioners feel stuck.
Not because the thyroid is confusing but because the thyroid is rarely the true starting point.
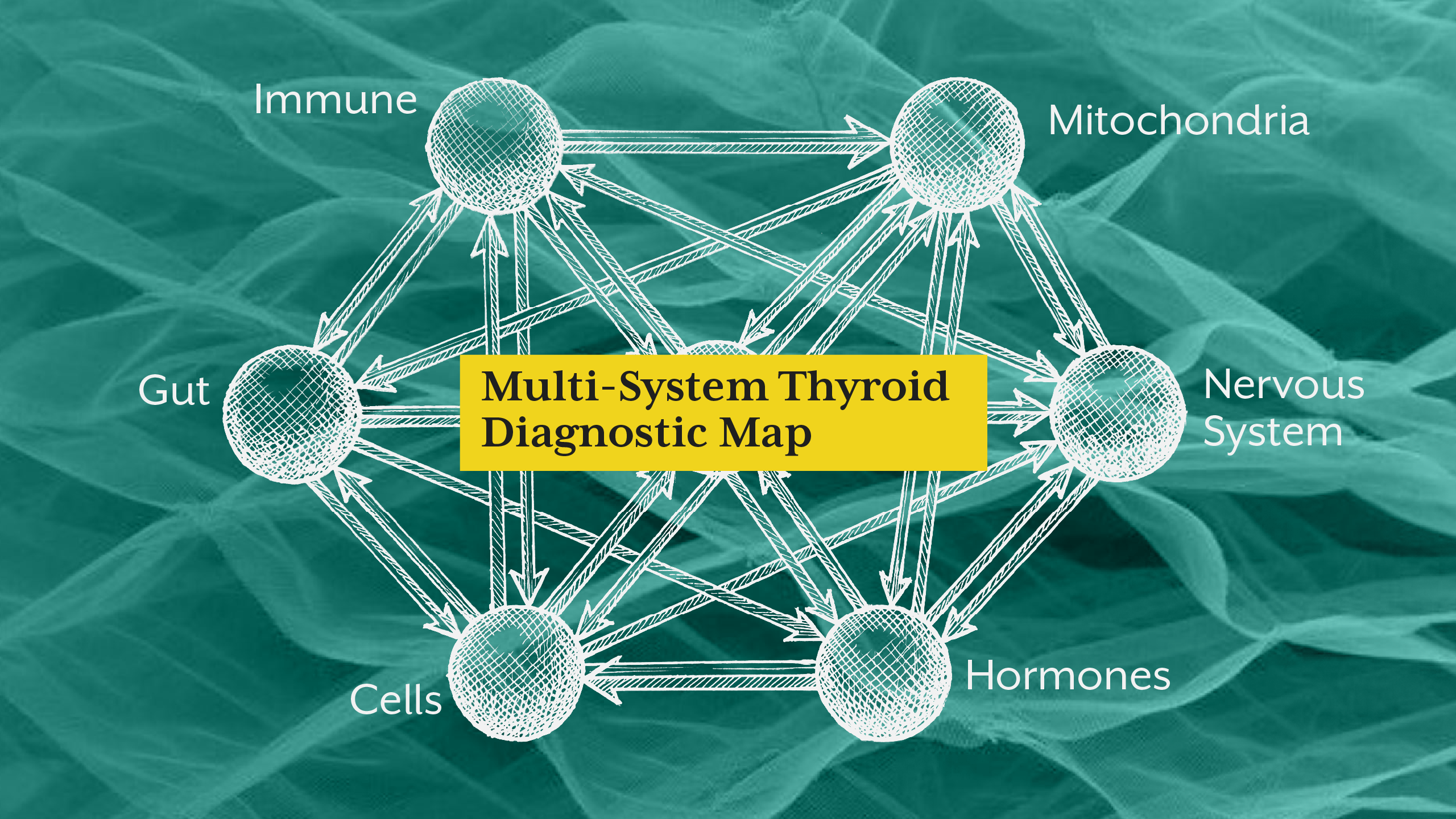
Clinical reality is far more complex than hormone replacement or lab normalization. What we are often observing is a multi-system regulatory disorder expressed through thyroid dysfunction. The thyroid becomes the visible endpoint of deeper physiological dysregulation involving immune signalling, mitochondrial energy production, gut permeability, autonomic nervous system balance, and cellular responsiveness.
If you are managing complex hormonal cases, you are not treating an endocrine gland in isolation. You are interpreting an integrated biological network.
This is where advanced case analysis begins.
As explored in “Hyperinsulinemia in Clinical Practice: The Most Under-Recognized Driver of Type 2 Diabetes”, disease processes often begin long before diagnostic labels appear. Thyroid dysfunction follows a similar trajectory which is progressive, systemic, and often invisible until regulatory capacity fails.
To interpret complex thyroid disorders accurately, practitioners must move beyond single-system thinking and adopt structured multi-system diagnostics.
Section 1 - Why Conventional Thyroid Case Analysis Falls Short
Traditional thyroid evaluation is reductionist by design. It focuses on hormone quantity rather than hormone context.
Clinical training typically emphasizes:
- Hormone production
- Hormone replacement
- Lab normalization
What it does not systematically evaluate is regulatory coherence across physiological systems.
You may have encountered cases where thyroid hormone levels appear “normal,” yet patients report persistent fatigue, weight changes, temperature intolerance, mood instability, or cognitive dysfunction. These are not diagnostic errors, rather they are regulatory mismatches.
Hormones function as signalling molecules. Their effectiveness depends not only on presence, but also on transport, conversion, receptor sensitivity, cellular energy availability, and inflammatory environment.
When these layers are ignored, treatment becomes partial by definition.
This is why many cases labelled “treatment-resistant hypothyroidism” are actually system-resistant physiology.
Section 2 - The Gut-Immune Axis in Thyroid Case Complexity
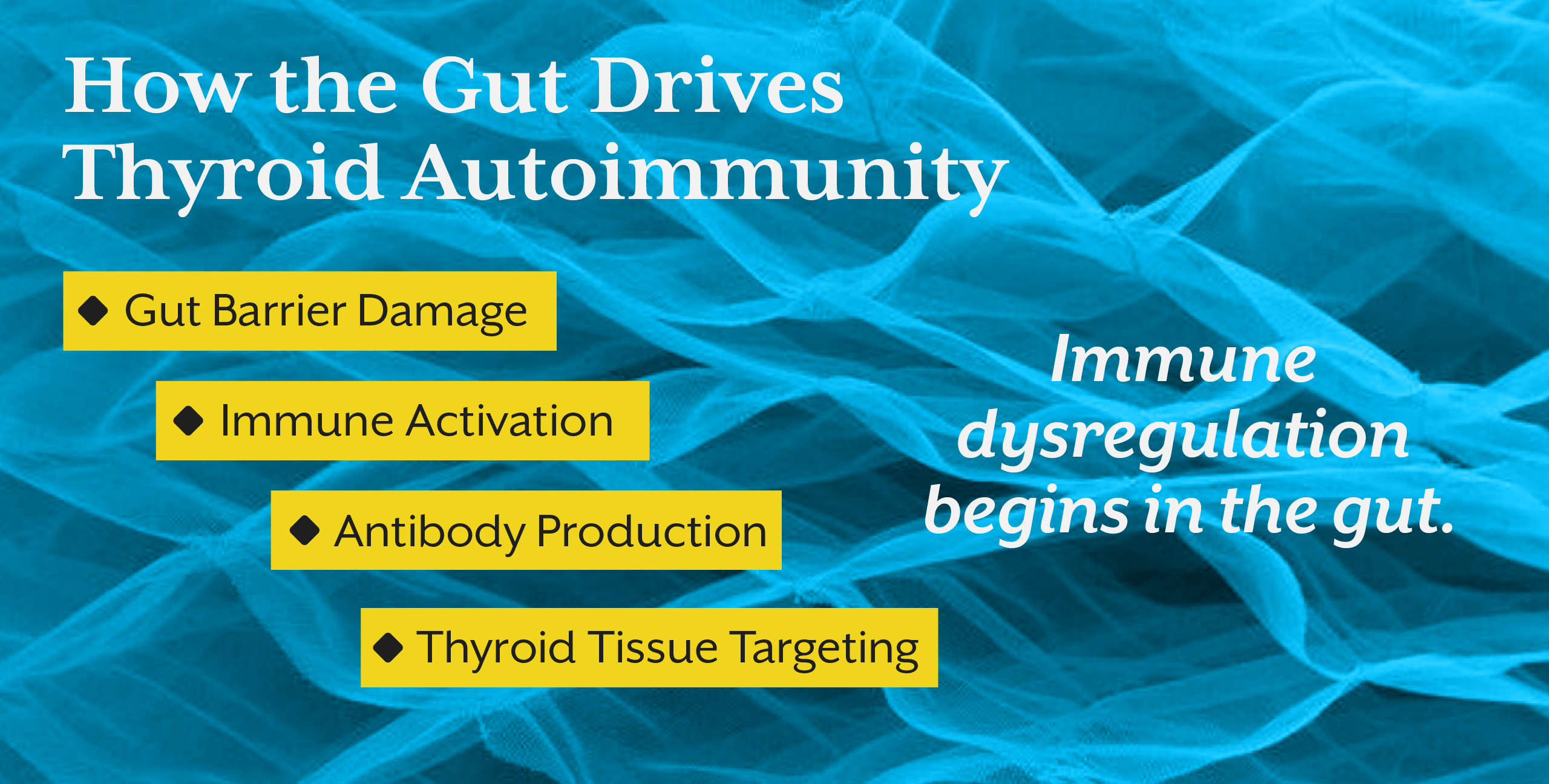
Many complex thyroid cases are fundamentally immune-driven.
Autoimmune thyroid disorders do not emerge spontaneously. They arise from immune dysregulation, which is frequently rooted in intestinal barrier dysfunction and chronic antigen exposure.
The gut is not simply a digestive organ. It is the largest immune interface in the body. When barrier integrity declines, immune activation increases. Cytokine signalling intensifies. Molecular mimicry becomes more likely. Autoimmune reactivity escalates.
In clinical practice, this often manifests as fluctuating thyroid antibody levels, unpredictable symptom severity, and inconsistent treatment response.
You may stabilize hormone levels, yet inflammatory signalling continues to interfere with cellular responsiveness.
This is why structural gut assessment becomes essential in advanced thyroid case analysis.
A similar systemic model is discussed in “Insulin Resistance as a Pre-Diagnostic State: Why Type 2 Diabetes Is a Late Clinical Label.” Just as metabolic dysfunction precedes diabetes, immune dysregulation often precedes thyroid autoimmunity.
The thyroid is not initiating the disorder, it is participating in a wider immune narrative.
Section 3 - Mitochondrial Function Determines Hormonal Impact
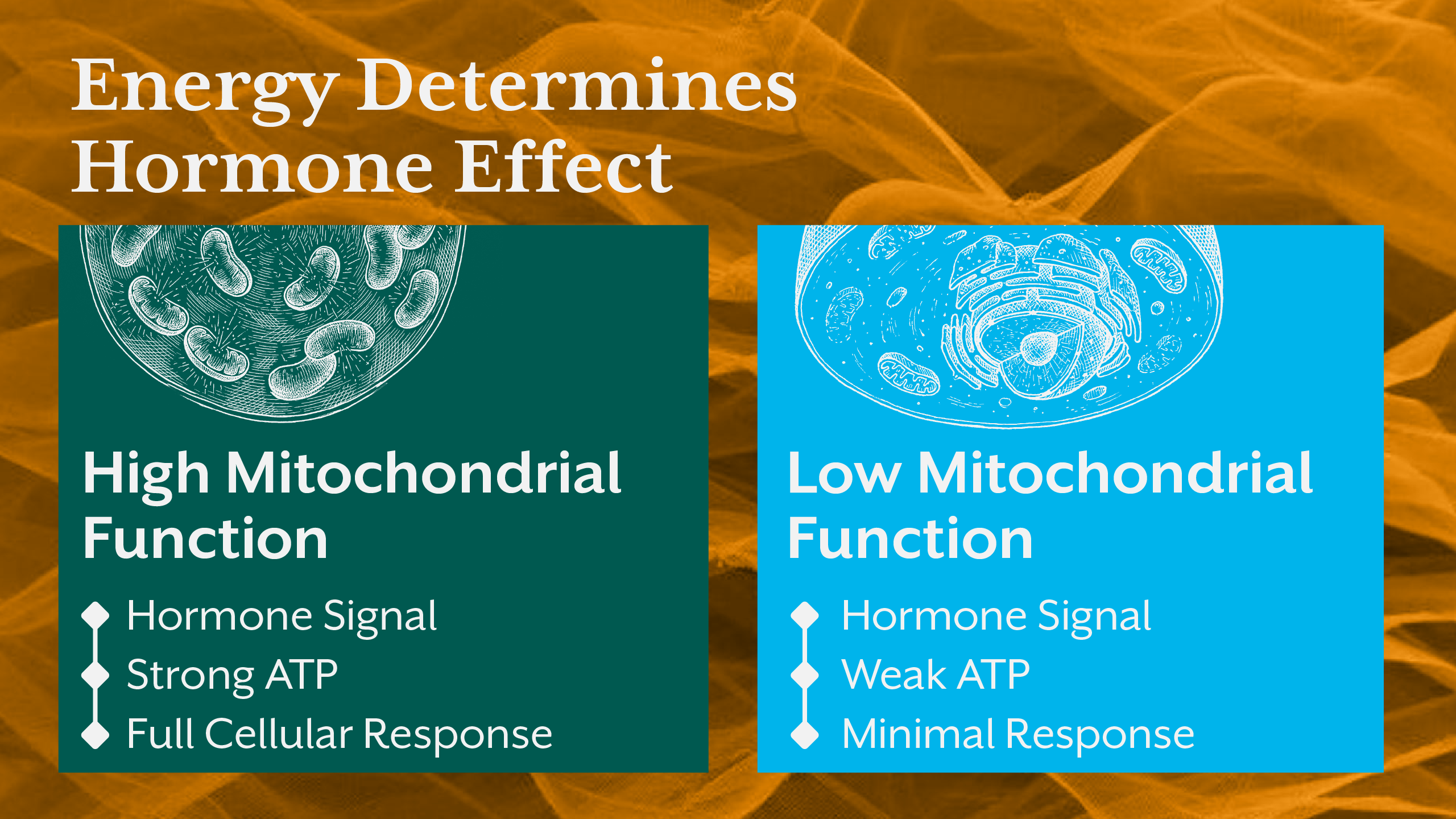
Hormones regulate metabolic activity. Mitochondria execute it.
This distinction is critical.
Thyroid hormones increase cellular energy demand. They stimulate oxygen consumption, ATP production, and metabolic turnover. But if mitochondrial function is impaired, cells cannot respond adequately regardless of hormone availability.
Clinically, this creates a paradox.
Hormone levels appear sufficient. Yet metabolic output remains suppressed.
Patients describe persistent fatigue, poor exercise tolerance, cognitive slowing, and impaired thermoregulation, classic low-metabolism symptoms even when thyroid hormone levels fall within reference ranges.
What you are observing is not hormonal deficiency, but energetic incapacity.
Mitochondrial dysfunction alters receptor responsiveness, reduces intracellular signalling efficiency, and limits physiological adaptation. The endocrine signal arrives. The cell cannot execute the instruction.
This is why energy metabolism assessment is indispensable in advanced thyroid case work.
Section 4 - Nervous System Regulation and Hormonal Adaptation
One of the most overlooked factors in thyroid case analysis is autonomic nervous system regulation.
Hormonal systems do not function independently of neural control. Chronic stress, sympathetic dominance, and disrupted circadian rhythms significantly alter endocrine signalling.
Persistent stress elevates cortisol, shifts metabolic priorities, impairs peripheral hormone conversion, and modifies receptor sensitivity. Over time, this produces adaptive metabolic suppression, a protective mechanism against sustained physiological strain.
Patients experiencing chronic stress frequently show:
- Hormone conversion inefficiency
- Blunted metabolic response
- Altered appetite regulation
- Fat distribution changes
This explains why thyroid dysfunction often coexists with weight regulation challenges and stress-related metabolic patterns.
You are not observing endocrine failure alone. You are observing neuroendocrine adaptation.
Section 5 - Building a Structured Multi-System Diagnostic Model
When practitioners encounter complex thyroid cases, the challenge is not identifying dysfunction, it is organizing complexity.
A systematic clinical framework must evaluate:
- Hormone production and transport
- Immune activation patterns
- Gut integrity and microbial signalling
- Mitochondrial energy capacity
- Nervous system regulation
- Cellular responsiveness
Each domain influences the others. No single intervention resolves systemic dysregulation if other regulatory layers remain unstable.
This integrative clinical reasoning is central to training within iThrive Academy and forms the structural foundation of iThrive Certified Functional Nutrition (iCFN).
For practitioners seeking focused thyroid specialization, the Certified Thyroid Educator program teaches structured assessment of hormonal signalling within whole-system physiology.
The goal is not more testing. The goal is meaningful interpretation.
Key Takeaway
Advanced thyroid case analysis is not about identifying which hormone is abnormal, it is about understanding why regulatory coordination has failed. Complex thyroid disorders emerge when multiple physiological systems lose synchrony: immune signalling becomes reactive, mitochondrial energy production declines, nervous system regulation shifts toward chronic stress adaptation, and gut-mediated immune activation intensifies. The thyroid reflects this systemic imbalance rather than causing it independently. When practitioners learn to evaluate these interconnected domains through structured multi-system diagnostics, treatment becomes precise, adaptive, and physiologically coherent. The future of thyroid care is not gland-focused, rather it is systems-focused.






.jpg)